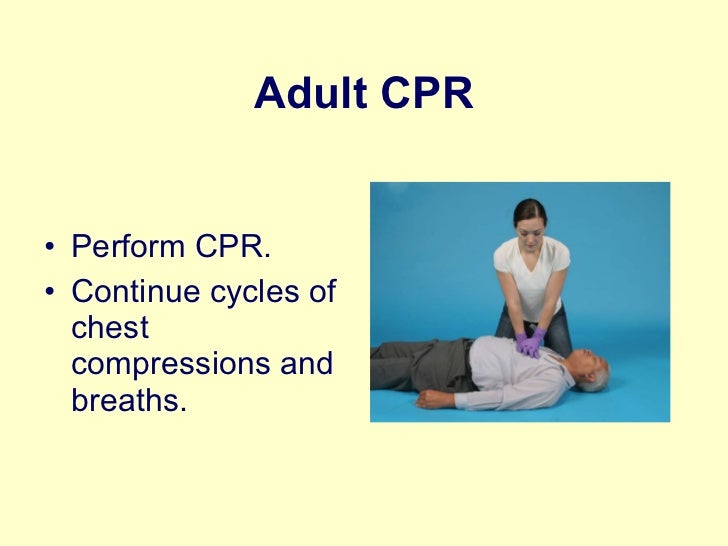
Continue Cpr
Press Z to toggle the console. Feel the snow console commands.
Giving CPR for More Than 30 Minutes May Be Worth It. Study finds keeping resuscitation efforts going for longer could improve brain function in survivors. From the WebMD Archives.
CPR stands for cardiopulmonary resuscitation. It is a lifesaving procedure that is done when someone's breathing or heartbeat has stopped. This may happen after an, drowning, or heart attack. CPR involves:.
Rescue breathing, which provides oxygen to a person's lungs. Chest compressions, which keep the person's blood circulating.Permanent brain damage or death can occur within minutes if a person's blood flow stops. Therefore, you must continue CPR until the person's heartbeat and breathing return, or trained medical help arrives.For the purposes of CPR, puberty is defined as breast development in females and the presence of axillary (armpit) hair in males. CPR is best done by someone trained in an accredited CPR course. The procedures described here are NOT a substitute for CPR training. The newest techniques emphasize compression over rescue breathing and airway management, reversing a long-standing practice.
See for classes near you.Time is very important when an person is not breathing. Permanent brain damage begins after only 4 minutes without oxygen, and death can occur as soon as 4 to 6 minutes later.Machines called automated external defibrillators (AEDs) can be found in many public places, and are available for home use. These machines have pads or paddles to place on the chest during a life-threatening emergency. They automatically check the heart rhythm and give a sudden shock if, and only if, that shock is needed to get the heart back into the right rhythm. When using an AED, follow the instructions exactly.
In adults, major reasons that heartbeat and breathing stop include:. Drug overdose.
Excessive bleeding. Heart problem (heart attack or abnormal heart rhythm, fluid in the lungs or compressing the heart).
Infection in the bloodstream. Injuries and accidents. Drowning. StrokeThere are many things that cause an older child or teen's heartbeat and breathing to stop, including:. Choking. Drowning. Electrical shock.
Excessive bleeding. Head trauma or other serious injury. Lung disease. Poisoning.
Suffocation. Check for responsiveness. Shake or tap the person gently. See if the person moves or makes a noise. Shout, 'Are you OK?'
Call 911 if there is no response. Shout for help and send someone to call 911. If you are alone, call 911 and retrieve an AED (if available), even if you have to leave the person.3. Carefully place the person on their back. If there is a chance the person has a spinal injury, two people should move the person to prevent the head and neck from twisting.4. Perform chest compressions:.
Place the heel of one hand on the breastbone - right between the nipples. Place the heel of your other hand on top of the first hand. Position your body directly over your hands. Give 30 chest compressions. These compressions should be fast and hard. Press down about 2 inches (5 centimeters) into the chest. Each time, let the chest rise completely.
Count the 30 compressions quickly: '1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30, off'.5. Open the airway. Lift up the chin with 2 fingers. At the same time, tilt the head by pushing down on the forehead with the other hand.6. Look, listen, and feel for breathing. Place your ear close to the person's mouth and nose.
Watch for chest movement. Feel for breath on your cheek.7. If the person is not breathing or has trouble breathing:.
Cover their mouth tightly with your mouth. Pinch the nose closed. Keep the chin lifted and head tilted. Give 2 rescue breaths. Each breath should take about a second and make the chest rise.8.
Repeat chest compressions and rescue breathing until the person recovers or help arrives. If an AED for adults is available, use it as soon as possible.If the person starts breathing again, place them in the recovery position. Keep checking for breathing until help arrives.
In adults, to avoid injuries and heart problems that can lead to the heart stopping beating:. Eliminate or reduce risk factors that contribute to heart disease, such as cigarette smoking, high cholesterol, high blood pressure, obesity, and stress. Get plenty of exercise. See your health care provider regularly. Always use seat belts and drive safely. Avoid using illegal drugs.Most children need CPR because of a preventable accident.
The following tips may help prevent some accidents in children:. Teach your children the basic principles of family safety. Teach your child to swim. Teach your child to watch for cars and ride bikes safely. Teach your child firearm safety. If you have guns in your home, keep them locked in an isolated cabinet. American Heart Association.
Highlights of the 2015 American Heart Association guidelines update for CPR and ECC. Accessed March 14, 2019.Duff JP, Topjian A, Berg MD, et al. 2018 American Heart Association focused update on pediatric advanced life support: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. PMID: 30571264.Morley PT. Cardiopulmonary resuscitation (including defibrillation).
In: Bersten AD, Handy JM, eds. Oh's Intensive Care Manual. Philadelphia, PA: Elsevier; 2019:chap 21.Panchal AR, Berg KM, Kudenchuk PJ, et al. 2018 American Heart Association focused update on advanced cardiovascular life support use of antiarrhythmic drugs during and immediately after cardiac arrest: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.
PMID: 30571262. For Health Content Provider (www.urac.org).
URAC's is an independent audit to verify that A.D.A.M. Follows rigorous standards of quality and accountability.
Is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.' Is also a founding member of Hi-Ethics.
This site complies with the HONcode standard for trustworthy health information:.The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only - they do not constitute endorsements of those other sites. Copyright 1997-2020, A.D.A.M., Inc. Duplication for commercial use must be authorized in writing by ADAM Health Solutions.
It's far better to do something than to do nothing at all if you're fearful that your knowledge or abilities aren't 100 percent complete. Remember, the difference between your doing something and doing nothing could be someone's life.Here's advice from the American Heart Association:. Untrained. If you're not trained in CPR, then provide hands-only CPR.
That means uninterrupted chest compressions of 100 to 120 a minute until paramedics arrive (described in more detail below). You don't need to try rescue breathing. Trained and ready to go. If you're well-trained and confident in your ability, check to see if there is a pulse and breathing. If there is no breathing or a pulse within 10 seconds, begin chest compressions. Start CPR with 30 chest compressions before giving two rescue breaths.
Trained but rusty. If you've previously received CPR training but you're not confident in your abilities, then just do chest compressions at a rate of 100 to 120 a minute.
(Details described below.)The above advice applies to adults, children and infants needing CPR, but not newborns (infants up to 4 weeks old).CPR can keep oxygenated blood flowing to the brain and other vital organs until more definitive medical treatment can restore a normal heart rhythm.When the heart stops, the lack of oxygenated blood can cause brain damage in only a few minutes. A person may die within eight to 10 minutes.To learn CPR properly, take an accredited first-aid training course, including CPR and how to use an automated external defibrillator (AED). If you are untrained and have immediate access to a phone, call 911 or your local emergency number before beginning CPR. The dispatcher can instruct you in the proper procedures until help arrives. Before you beginBefore starting CPR, check:.
Is the environment safe for the person?. Is the person conscious or unconscious?. If the person appears unconscious, tap or shake his or her shoulder and ask loudly, 'Are you OK?' . If the person doesn't respond and two people are available, have one person call 911 or the local emergency number and get the AED, if one is available, and have the other person begin CPR.
If you are alone and have immediate access to a telephone, call 911 or your local emergency number before beginning CPR. Get the AED, if one is available. As soon as an AED is available, deliver one shock if instructed by the device, then begin CPR. Chest compressionsTo perform chest compressions, kneel next to the person's neck and shoulders.
Place the heel of one hand over the center of the person's chest and your other hand on top. Keep your elbows straight and position your shoulders directly above your hands. Using your upper body weight, push straight down on the chest about 2 inches, or 5 centimeters, but not more than 2.4 inches, or 6 centimeters. Push hard at a rate of 100 to 120 compressions a minute. If you haven't been trained in CPR, continue chest compressions until there are signs of movement or until emergency medical personnel take over. If you have been trained in CPR, go on to opening the airway and rescue breathing.
Rescue breathingWith the airway open (using the head-tilt, chin-lift maneuver), pinch the nostrils shut for mouth-to-mouth breathing and cover the person's mouth with yours, making a seal. Give the first rescue breath, lasting one second, and watch to see if the chest rises. If it does rise, give the second breath. If the chest doesn't rise, repeat the head-tilt, chin-lift maneuver and then give the second breath. After this, start chest compressions again to restore circulation. Thirty chest compressions followed by two rescue breaths is considered one cycle.
Be careful not to provide too many breaths or to breathe with too much force.The American Heart Association uses the letters C-A-B — compressions, airway, breathing — to help people remember the order to perform the steps of CPR. Compressions: Restore blood circulation. Put the person on his or her back on a firm surface.
Kneel next to the person's neck and shoulders. Place the heel of one hand over the center of the person's chest, between the nipples. Place your other hand on top of the first hand. Keep your elbows straight and position your shoulders directly above your hands. Use your upper body weight (not just your arms) as you push straight down on (compress) the chest at least 2 inches (approximately 5 centimeters) but not greater than 2.4 inches (approximately 6 centimeters). Push hard at a rate of 100 to 120 compressions a minute. If you haven't been trained in CPR, continue chest compressions until there are signs of movement or until emergency medical personnel take over.
If you have been trained in CPR, go on to opening the airway and rescue breathing.Airway: Open the airway. If you're trained in CPR and you've performed 30 chest compressions, open the person's airway using the head-tilt, chin-lift maneuver. Put your palm on the person's forehead and gently tilt the head back. Then with the other hand, gently lift the chin forward to open the airway. Breathing: Breathe for the personRescue breathing can be mouth-to-mouth breathing or mouth-to-nose breathing if the mouth is seriously injured or can't be opened. With the airway open (using the head-tilt, chin-lift maneuver), pinch the nostrils shut for mouth-to-mouth breathing and cover the person's mouth with yours, making a seal.
Prepare to give two rescue breaths. Give the first rescue breath — lasting one second — and watch to see if the chest rises. If it does rise, give the second breath. If the chest doesn't rise, repeat the head-tilt, chin-lift maneuver and then give the second breath.
Thirty chest compressions followed by two rescue breaths is considered one cycle. Be careful not to provide too many breaths or to breathe with too much force. Resume chest compressions to restore circulation. As soon as an automated external defibrillator (AED) is available, apply it and follow the prompts. Administer one shock, then resume CPR — starting with chest compressions — for two more minutes before administering a second shock.
If you're not trained to use an AED, a 911 or other emergency medical operator may be able to guide you in its use. If an AED isn't available, go to step 5 below.
Continue CPR until there are signs of movement or emergency medical personnel take over. If you're alone and you did see the child collapse, call 911 or your local emergency number and get the AED, if one is available, before beginning CPR.
If another person is available, have that person call for help and get the AED while you begin CPR. Put the child on his or her back on a firm surface. Kneel next to the child's neck and shoulders. Use two hands, or only one hand if the child is very small, to perform chest compressions. Press straight down on (compress) the chest about 2 inches (approximately 5 centimeters).
If the child is an adolescent, push straight down on the chest at least 2 inches (approximately 5 centimeters) but not greater than 2.4 inches (approximately 6 centimeters). Push hard at a rate of 100 to 120 compressions a minute.
If you haven't been trained in CPR, continue chest compressions until there are signs of movement or until emergency medical personnel take over. If you have been trained in CPR, go on to opening the airway and rescue breathing.Airway: Open the airway. If you're trained in CPR and you've performed 30 chest compressions, open the child's airway using the head-tilt, chin-lift maneuver. Put your palm on the child's forehead and gently tilt the head back. Then with the other hand, gently lift the chin forward to open the airway.Breathing: Breathe for the childUse the same compression-breath rate that is used for adults: 30 compressions followed by two breaths.
This is one cycle. With the airway open (using the head-tilt, chin-lift maneuver), pinch the nostrils shut for mouth-to-mouth breathing and cover the child's mouth with yours, making a seal. Prepare to give two rescue breaths. Give the first rescue breath — lasting one second — and watch to see if the chest rises. If it does rise, give the second breath.
If the chest doesn't rise, repeat the head-tilt, chin-lift maneuver and then give the second breath. Be careful not to provide too many breaths or to breathe with too much force. After the two breaths, immediately begin the next cycle of compressions and breaths. If there are two people performing CPR, conduct 15 compressions followed by two breaths.
As soon as an AED is available, apply it and follow the prompts. Use pediatric pads if available, for children up to age 8. If pediatric pads aren't available, use adult pads. Administer one shock, then resume CPR — starting with chest compressions — for two more minutes before administering a second shock. If you're not trained to use an AED, a 911 or other emergency medical operator may be able to guide you in its use.Continue until the child moves or help arrives. If there's no response, follow the C-A-B procedures below for a baby under age 1 (except newborns, which includes babies up to 4 weeks old) and time the call for help as follows:.
If you're the only rescuer and you didn't see the baby collapse, do CPR for two minutes — about five cycles — before calling 911 or your local emergency number and getting the AED. If you did see the baby collapse, call 911 or your local emergency number and get the AED, if one is available, before beginning CPR. If another person is available, have that person call for help immediately and get the AED while you attend to the baby.Compressions: Restore blood circulation. Place the baby on his or her back on a firm, flat surface, such as a table. The floor or ground also will do.
Imagine a horizontal line drawn between the baby's nipples. Place two fingers of one hand just below this line, in the center of the chest.
Gently compress the chest about 1.5 inches (about 4 centimeters). Count aloud as you pump in a fairly rapid rhythm.
You should pump at a rate of 100 to 120 compressions a minute.Airway: Open the airway. After 30 compressions, gently tip the head back by lifting the chin with one hand and pushing down on the forehead with the other hand.Breathing: Breathe for the baby.
Cover the baby's mouth and nose with your mouth. Prepare to give two rescue breaths. Use the strength of your cheeks to deliver gentle puffs of air (instead of deep breaths from your lungs) to slowly breathe into the baby's mouth one time, taking one second for the breath. Watch to see if the baby's chest rises. If it does, give a second rescue breath. If the chest does not rise, repeat the head-tilt, chin-lift maneuver and then give the second breath. If the baby's chest still doesn't rise, continue chest compressions.
Give two breaths after every 30 chest compressions. If two people are conducting CPR, give two breaths after every 15 chest compressions. Perform CPR for about two minutes before calling for help unless someone else can make the call while you attend to the infant. Continue CPR until you see signs of life or until medical personnel arrive. Field JM, et al. Part 1: Executive summary — 2017 update. American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care.
Accessed Dec. 8, 2017. Pozner CN. Basic life support (BLS) in adults. Accessed Dec. 8, 2017. Highlights of the 2015 American Heart Association guidelines update for CPR and ECC.
American Heart Association. Accessed Dec. 10, 2017.
Neumar RW, et al. Part 1: Executive summary 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. 2015;132(suppl 2):S315. Atkins DL, et al. 2017 American Heart Association focused update on pediatric basic life support and cardiopulmonary resuscitation quality: An update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.
2018;137:e1. Torrey SB.
Pediatric basic life support for health care providers. Accessed Dec. 14, 2017.
Part 11: Pediatric basic life support and cardiopulmonary resuscitation quality. American Heart Association. Accessed Dec. 13, 2017. Dorland's Illustrated Medical Dictionary. Philadelphia, Pa.: W.B.
Saunders; 2011. Accessed Feb.